Contents
Telemedicine has evolved from an optional digital service into a core healthcare delivery channel. The growing adoption reflects both patient demand for remote care and provider needs to improve access, efficiency, and continuity of care.
According to Grand View Research, the global telemedicine market generated $141.19 billion in 2024 and is projected to reach $380.33 billion by 2030, highlighting how rapidly virtual care is becoming mainstream across healthcare ecosystems.
As this growth accelerates, healthcare providers, hospitals, startups, and digital health companies are investing in telemedicine platforms that go far beyond basic video consultations. Modern telemedicine platform development requires careful planning around regulatory compliance, data security, interoperability, scalability, and performance.
Decisions related to architecture, integrations with EHR systems, payment processing, and remote monitoring directly impact clinical outcomes, patient experience, and long-term platform sustainability. Working with experienced medical practice management software development partners ensures these telemedicine platforms seamlessly integrate with existing practice management workflows, enabling unified scheduling, billing, documentation, and reporting across both in-person and virtual care delivery models for a comprehensive patient care ecosystem.
This guide breaks down everything you need to know about telemedicine platform development, including essential features, technology stack considerations, development workflows, cost factors, and best practices. Drawing from our experience as a leading telemedicine platform development agency, we’ve shared insights on what it takes to build a successful telemedicine platform that improves patient care and healthcare workflows.
What is Telemedicine Platform Development?
Telemedicine platform development is the process of designing, building, and deploying a secure digital system that enables healthcare providers to deliver medical services remotely. These platforms support virtual consultations, patient data management, digital prescriptions, payments, and ongoing care coordination through web and mobile applications.
Unlike standalone video calling tools, a telemedicine platform is a comprehensive healthcare solution. It combines real-time communication technologies with backend systems that manage patient records, appointment scheduling, clinical workflows, and integrations with third-party healthcare systems such as EHRs, pharmacy networks, and diagnostic tools.
The goal is to replicate and enhance in-person care while maintaining compliance with healthcare regulations and data privacy standards.
A well-developed telemedicine platform typically includes role-based access for patients, providers, and administrators, along with features such as secure video conferencing, chat and file sharing, e-prescriptions, billing, and analytics. On the backend, it relies on scalable cloud infrastructure, encrypted data storage, APIs for system interoperability, and monitoring tools to ensure performance and reliability.
Types of telemedicine solutions
Healthcare organizations can choose from several telemedicine platform types based on their specific needs and patient populations.
1. Synchronous telemedicine
Enables real-time video consultations between patients and providers. This model works well for primary care visits, mental health sessions, and urgent care consultations. It requires robust video streaming infrastructure and low-latency connections.
2. Asynchronous telemedicine
Uses store-and-forward technology for non-urgent consultations. Patients submit photos, medical history, and symptoms through secure portals. Dermatology and radiology practices commonly use this approach for diagnostic reviews.
3. Remote patient monitoring
Platforms collect health data from connected devices continuously. These solutions track vital signs, blood glucose levels, and other metrics in real time. Chronic disease management programs benefit significantly from this technology.
4. Hybrid telemedicine platforms
Combine multiple delivery modes within a single solution. This approach offers flexibility for healthcare organizations serving diverse patient populations. Most enterprise healthcare systems prefer this comprehensive model.
Why Invest in Custom Telemedicine Platform Development?
Healthcare organizations face a critical decision when implementing virtual care capabilities. They can choose off-the-shelf solutions or invest in custom telemedicine development. Understanding the advantages of custom development helps organizations make informed decisions.
1. Competitive differentiation in a crowded market
The telehealth market has become increasingly competitive since 2020. According to the American Medical Association, 71.4% of physicians now use telehealth weekly, up from just 25.1% in 2018. Standing out requires unique features and superior patient experiences.
Custom platforms allow you to implement specialty-specific workflows that generic solutions cannot match. A mental health practice needs features different from those of a dermatology clinic. Custom development ensures your platform aligns perfectly with your clinical workflows.
2. Seamless integration with existing healthcare systems
Healthcare organizations operate complex technology ecosystems with EHR systems, billing platforms, and practice management software. Custom telemedicine solutions integrate directly with these existing systems without disruptive workarounds.
Epic EHR integration development and Cerner integration represent common requirements for hospital systems. According to TechMagic, 84% of hospitals now use HL7 FHIR APIs for healthcare data exchange. Custom platforms leverage these standards for seamless interoperability.
3. Full ownership and control
White-label telemedicine solutions come with ongoing licensing fees and limited customization options. Custom platform development provides full ownership of your intellectual property. You control the roadmap, features, and scaling decisions without vendor dependencies.
This ownership model proves particularly valuable for healthcare startups seeking investment. Investors prefer companies with proprietary technology assets to those that depend on third-party platforms.
4. Scalability for future growth
Healthcare organizations often start with basic telehealth capabilities and expand over time. Custom architecture lets you add features, users, and specialties without migrating to a different platform. This scalability protects your initial investment as your virtual care program grows.
Scale Virtual Care With Custom Telemedicine Platform Development
Empower providers with scalable telemedicine platforms designed for high availability, data security, smooth patient experiences, and compliance with global healthcare regulations.

Core Features of a Telemedicine Platform
Successful telemedicine platforms require specific features to deliver quality virtual care experiences. The feature set varies based on your target users and healthcare specialty. However, certain capabilities remain essential across all telemedicine applications.
1. Patient-facing features
Your patients interact with the platform most frequently. Their experience determines adoption rates and satisfaction scores.
1.1 User registration and profile management
Patients need simple onboarding with secure identity verification. Medical history collection forms should capture relevant information without overwhelming users. Profile management allows patients to update insurance, contact details, and preferences.
1.2 Appointment scheduling and calendar integration
Intuitive scheduling interfaces show provider availability in real time. Calendar integration automatically syncs appointments with patient smartphones. Automated reminders via SMS and email significantly reduce no-show rates.
1.3 Secure video consultation interface
High-definition video streaming ensures clear communication during consultations. Features like screen sharing, virtual waiting rooms, and in-call chat enhance the experience. Mobile-optimized interfaces accommodate patients using smartphones and tablets.
1.4 Prescription and documentation access
Patients should be able to easily access electronic prescriptions, lab orders, and consultation summaries. Secure document storage allows patients to review their medical records anytime. Integration with pharmacy networks enables prescription delivery and pickup options.
1.5 Payment and insurance processing
Integrated payment gateways securely process copays and self-pay amounts. Insurance verification APIs confirm coverage before appointments. Clear cost estimates help patients understand their financial responsibility upfront.
2. Provider-facing features
Healthcare providers need efficient tools that seamlessly integrate into their clinical workflows. Provider satisfaction directly impacts platform adoption and patient care quality.
2.1 Dashboard and appointment management
Comprehensive dashboards clearly display daily schedules, pending tasks, and patient queues. Providers should start consultations, review patient histories, and access clinical tools from a single interface. Queue management features help practices handle high patient volumes efficiently.
2.2 Clinical documentation tools
Integrated note-taking tools streamline documentation during and after consultations. Pre-built templates accelerate charting for common visit types. Voice-to-text transcription reduces documentation burden for providers.
2.3 E-prescribing and medication management
Electronic prescription capabilities include drug interaction checking and formulary verification. Integration with pharmacy networks enables real-time prescription tracking. Controlled substance prescribing requires additional compliance features in certain states.
2.4 Referral and care coordination
Secure referral workflows connect patients with specialists within and outside your network. Care coordination tools track referral status and facilitate provider-to-provider communication. These features prove essential for integrated delivery networks and accountable care organizations.
3. Administrative features
Healthcare administrators require visibility into platform performance and operational metrics. Administrative tools support compliance monitoring, resource allocation, and financial management.
3.1 Analytics and reporting dashboards
Real-time analytics track consultation volumes, wait times, and revenue metrics. Custom reports support quality improvement initiatives and board presentations. Exportable data enables integration with business intelligence platforms.
3.2 User and access management
Role-based access controls ensure appropriate data access for different user types. Administrator tools manage provider credentials, scheduling rules, and patient access settings. Audit trails track all system access for compliance documentation.
3.3 Billing and revenue cycle management
Automated claim generation captures appropriate billing codes for telemedicine services. Integration with clearinghouses streamlines claim submission and payment posting. Revenue dashboards help administrators monitor financial performance across providers.
Get Expert Guidance on Feature Selection for Your Telemedicine Platform
Not sure which features to pick for your telemedicine solution? Our experts can help. Get a customized feature list, development roadmap, and quote from our team.
Technology Stack for Telemedicine Platform Development
Choosing the right technology stack impacts platform performance, security, and long-term maintainability. Healthcare applications require specific technologies that support regulatory compliance and scalability requirements.
Frontend development options
The frontend technology determines user experience across web and mobile interfaces. Healthcare applications must perform consistently across devices and connection speeds.
| Technology | Best For | Considerations |
| React Native | Cross-platform mobile apps | Single codebase for iOS and Android, faster development. |
| Flutter | Cross-platform with custom UI | Excellent performance, growing healthcare adoption. |
| Swift | Native iOS applications | Best iOS performance, required for Apple Watch integration. |
| Kotlin | Native Android applications | Modern Android development, excellent performance. |
| React.js | Web applications | Large ecosystem, excellent for complex interfaces. |
| Angular | Enterprise web portals | Strong typing, suitable for large development teams. |
Cross-platform frameworks like React Native significantly reduce development time and cost. Our team uses React Native development for many healthcare projects to accelerate time-to-market while maintaining quality.
Backend technologies
The backend architecture handles business logic, data processing, and third-party integrations. Healthcare backends require robust security measures and compliance-ready data handling.
- Node.js delivers excellent performance for real-time applications such as video consultations. Its event-driven architecture efficiently handles concurrent connections. Many modern healthcare platforms choose Node.js for API development.
- Python provides extensive libraries for healthcare data processing and analytics. Django and FastAPI frameworks significantly accelerate backend development. Python excels at integrating machine learning capabilities for clinical decision support.
- PHP with Laravel remains popular for healthcare web applications requiring rapid development. Laravel provides excellent security features and database abstraction. Many established healthcare organizations maintain PHP-based systems.
Database solutions
Healthcare applications require databases that handle sensitive patient data securely while supporting complex queries.
- PostgreSQL provides HIPAA-compliant data storage with robust encryption. Its relational structure suits healthcare data models well. PostgreSQL efficiently handles complex reporting queries for analytics.
- MongoDB provides flexibility for unstructured medical data, such as clinical notes and images. Its document model accommodates varying data structures across medical specialties. MongoDB scales horizontally for high-volume applications.
Video communication infrastructure
Real-time video consultation requires specialized infrastructure for reliable, secure communication.
- WebRTC provides the foundation for peer-to-peer video communication in browsers and mobile apps. This open standard eliminates the need for plugins for patients. WebRTC integration for telehealth requires careful implementation for quality and security.
- Twilio offers video API integration with HIPAA-compliant infrastructure. Its SDKs significantly accelerate video feature development. Twilio handles scaling concerns that would otherwise require significant engineering investment.
- Agora SDK now provides ultra-low-latency video streaming suitable for clinical applications. Its global network ensures consistent quality across geographic regions. Agora offers healthcare-specific features like virtual backgrounds and noise cancellation.
Cloud infrastructure
Healthcare cloud deployments require infrastructure providers with healthcare compliance certifications.
| Provider | Healthcare Features | Compliance |
| AWS | HIPAA-eligible services, healthcare partner ecosystem. | BAA available, HITRUST certified. |
| Microsoft Azure | Healthcare APIs, AI health insights. | BAA available, comprehensive compliance. |
| Google Cloud | Healthcare API, Cloud Healthcare data engine. | BAA available, HIPAA compliant. |
Looking for expert guidance on telemedicine technology choices? Our healthcare app development team helps you select the optimal stack for your requirements.
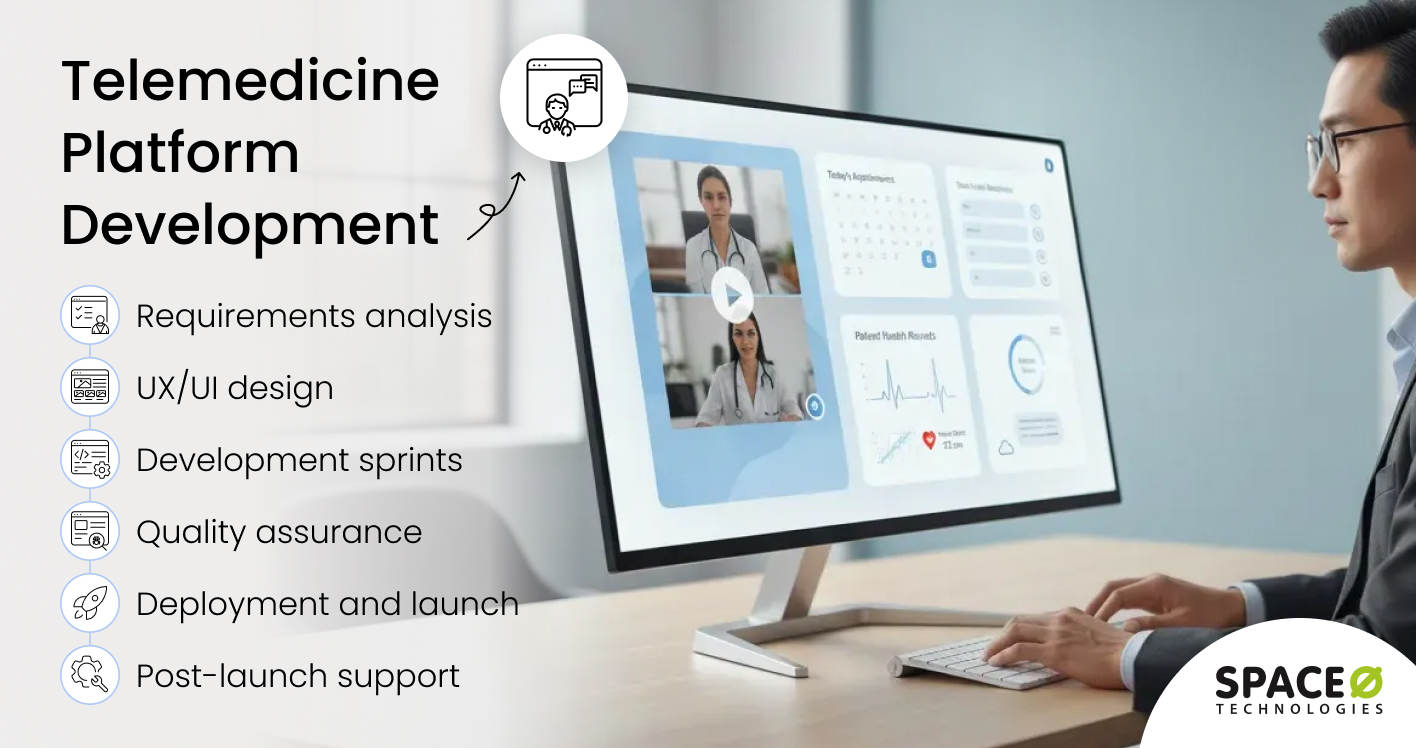
Step-by-Step Telemedicine Platform Development Process
Building a telemedicine platform requires a structured approach that addresses healthcare-specific requirements. The following process ensures successful delivery while managing regulatory and technical complexities.
Phase 1: Discovery and requirements analysis
The discovery phase establishes project foundations through stakeholder interviews and technical research. This phase typically spans 2-4 weeks, depending on project complexity.
- Stakeholder workshops: Engage clinicians, administrators, IT teams, and patient representatives in requirements gathering. Document clinical workflows that the platform must support. Identify pain points with existing systems and processes.
- Compliance requirements analysis: Map applicable regulations, including HIPAA, state telehealth laws, and payer requirements. Document data handling, storage, and transmission requirements. Identify required security controls and audit capabilities.
- Technical assessment: Evaluate existing healthcare IT infrastructure and integration requirements. Assess bandwidth and connectivity at clinical locations. Document EHR integration requirements and available APIs.
- Competitor and market research: Analyze competing solutions to identify opportunities for differentiation. Research patient preferences and adoption barriers. Document industry best practices for telemedicine user experience.
Phase 2: UX/UI design
Healthcare application design requires balancing clinical functionality with intuitive user experiences. Design sprints typically span 4-6 weeks for comprehensive platforms.
- User persona development: Create detailed personas for each user type, including patients, providers, and administrators. Document user goals, pain points, and technology proficiency levels. Use personas to guide design decisions throughout the project.
- Information architecture: Organize features and content into logical navigation structures. Map user journeys for critical workflows, such as scheduling and consultations. Design for accessibility compliance, including WCAG 2.1 guidelines.
- Wireframing and prototyping: Create low-fidelity wireframes for key screens and workflows. Develop interactive prototypes for usability testing with actual users. Iterate designs based on user feedback before development begins.
- Visual design: Develop brand-aligned visual designs that convey trust and professionalism. Create component libraries for consistent interface elements. Design responsive layouts that work across devices and screen sizes.
Phase 3: Development sprints
Agile development methodology works well for healthcare applications with evolving requirements. Development sprints typically span 2-3 weeks with regular stakeholder reviews.
- Sprint planning: Prioritize features based on clinical importance and technical dependencies. Break features into user stories with clear acceptance criteria. Estimate effort and assign work to development team members.
- Backend development: Build secure APIs that comply with healthcare data standards. Implement authentication, authorization, and audit logging. Develop integration connectors for EHR systems and external services.
- Frontend development: Build user interfaces based on approved designs. Implement responsive layouts and accessibility features. Develop video consultation interfaces with quality optimization in mind.
- Sprint reviews and retrospectives: Demonstrate completed features to stakeholders at the end of every sprint. Gather feedback and adjust priorities as needed. Continuously improve development processes based on team learnings.
You can partner with an expert healthcare software development company, like Space-O Technologies, to build your telemedicine solution. Such agencies bring years of healthcare domain experience and expertise to build your solution with zero technical hassle.
Phase 4: Quality assurance and testing
Healthcare applications require comprehensive testing to ensure patient safety and regulatory compliance. Testing phases typically overlap with development in agile projects.
- Functional testing: Verify all features work according to specifications. Test edge cases and error handling thoroughly. Validate business logic for clinical workflows.
- Security testing: Conduct penetration testing to identify vulnerabilities. Verify encryption implementation for data at rest and in transit. Test access controls and authentication mechanisms.
- Performance testing: Load test the video infrastructure under peak usage scenarios. Measure response times for critical operations. Identify and optimize performance bottlenecks.
- Compliance validation: Verify HIPAA technical safeguard implementation. Document security controls for audit purposes. Conduct risk assessments as required by regulations.
Phase 5: Deployment and launch
Careful deployment planning ensures smooth transitions to production environments. Launch phases include technical deployment and organizational change management.
- Infrastructure provisioning: Deploy cloud infrastructure in accordance with security best practices. Configure monitoring, alerting, and backup systems. Implement disaster recovery capabilities.
- Data migration: Securely migrate patient data from existing systems. Validate data integrity after migration. Document data lineage for compliance purposes.
- User training: Develop training materials for providers, staff, and administrators. Conduct hands-on training sessions before launch. Establish support resources for post-launch questions.
- Phased rollout. Launch to pilot groups before full deployment. Monitor system performance and user adoption closely. Address issues before expanding to additional users.
Phase 6: Post-launch support and optimization
Telemedicine platforms require ongoing maintenance and continuous improvement after launch. Support activities ensure long-term platform success and user satisfaction.
- Technical support: Provide help desk support for user questions and issues. Monitor system health and address incidents promptly. Apply security patches and platform updates regularly.
- Performance optimization: Analyze usage patterns and optimize accordingly. Improve video quality and reduce latency based on real-world data. Scale infrastructure to accommodate growing user bases.
- Feature enhancement: Gather user feedback systematically for improvement ideas. Prioritize enhancements based on clinical and business value. Release new features through regular update cycles.
Build a Patient-Centric Telemedicine Platform With Our Experts
Accelerate telemedicine platform development using proven frameworks, cloud-native architecture, and experienced healthcare developers focused on performance, security, and reliability.
Telemedicine App Development Cost Breakdown
Understanding the cost of telemedicine app development helps healthcare organizations budget appropriately for telemedicine initiatives. Costs vary significantly based on platform complexity, feature requirements, and development approach.
Cost estimates by platform type
The following estimates reflect typical development costs based on industry research and our project experience.
| Platform Type | Feature Set | Estimated Cost | Timeline |
| Basic MVP | Video calls, scheduling, and basic profiles. | $40,000 – $75,000 | 3-4 months |
| Standard Platform | Full scheduling, EHR integration, e-prescribing. | $100,000 – $200,000 | 5-8 months |
| Enterprise Solution | Multi-specialty, RPM, AI features, full integrations. | $250,000 – $500,000+ | 9-15 months |
Custom telemedicine apps typically cost $40,000 to $100,000 for basic versions and $100,000 to $300,000+ for feature-rich solutions. These estimates align with our experience delivering healthcare applications.
Cost breakdown by development phase
Understanding how costs distribute across project phases helps with financial planning.
| Phase | Percentage of Budget | Activities |
| Discovery and Design | 15-20% | Requirements, UX research, UI design, prototyping. |
| Development | 50-60% | Backend, frontend, integrations, video infrastructure. |
| Testing and QA | 15-20% | Functional, security, performance, and compliance testing. |
| Deployment and Launch | 5-10% | Infrastructure, migration, training, and go-live support. |
Ongoing operational costs
Budget for ongoing costs beyond initial development to maintain platform operations effectively.
- Infrastructure costs: Cloud hosting, video streaming, and storage incur monthly charges. Expect $2,000- $15,000 per month, depending on user volume and video usage.
- Maintenance and support: Bug fixes, security updates, and technical support require ongoing investment. Budget 15-20% of the initial development cost annually for maintenance.
- Compliance and security. Annual security assessments, penetration testing, and compliance audits add costs. Healthcare organizations should budget $10,000 to $50,000 annually for compliance activities.
- Feature enhancements: Plan for continuous improvement based on user feedback and market evolution. Most healthcare organizations allocate an ongoing development budget for new features.
Cost factors that influence the development budget
Several factors determine the total investment required for telemedicine platform development.
- Feature complexity: Basic video consultation platforms cost less than comprehensive platforms with remote monitoring, AI diagnostics, and multi-specialty support. Each additional feature increases development time and cost.
- Integration requirements: EHR integration, payment processing, and pharmacy network connections add development complexity. Integration work often accounts for 20-30% of total project effort for healthcare applications.
- Compliance requirements: HIPAA compliance adds cost for security implementation, auditing, and documentation. Additional regulations, such as state-specific requirements, further increase compliance efforts.
- Platform coverage: Web-only platforms cost less than multi-platform solutions that cover iOS, Android, and the web. Cross-platform frameworks reduce costs compared to native development for each platform.
- Development team location: Hourly rates vary significantly by geographic region. Offshore development teams offer cost advantages while onshore teams provide easier communication.
The telemedicine software typically achieves 100% ROI within 6 months through reduced no-shows, increased appointment capacity, and operational efficiencies. Want a detailed cost estimate for your telemedicine project? Use our app cost calculator for a preliminary budget assessment.
Get a Customized Cost Estimate for Your Telemedicine Project
Share your requirements with our team for a detailed cost breakdown, pricing factors, and budgeting insights for building a telemedicine platform. NDA protection guaranteed.
Compliance and Security Requirements
Healthcare applications face stringent regulatory requirements that impact design, development, and operations. Non-compliance risks include significant financial penalties, legal liability, and reputational damage.
1. HIPAA compliance for telemedicine
The Health Insurance Portability and Accountability Act establishes requirements for protecting patient health information. Telemedicine platforms must implement specific technical, administrative, and physical safeguards.
1.1 Technical safeguards
Encryption requirements apply to data in transit and at rest. Access controls must enforce minimum necessary access principles. Audit controls must comprehensively track access to protected health information.
1.2 Administrative safeguards
Risk assessments must identify and address security vulnerabilities. Workforce training must cover privacy and security policies. Business associate agreements must cover all vendors handling patient data.
1.3 Physical safeguards
Device and media controls must properly address data disposal. Workstation security policies must protect access points. Facility access controls must limit physical access to systems.
2. Video consultation security
Secure video communication requires specific implementation considerations beyond general security practices.
2.1 End-to-end encryption
Video streams must use encryption that prevents interception during transmission. WebRTC provides encryption by default when implemented correctly. Third-party video APIs must offer HIPAA-compliant encryption options.
2.2 Recording policies
Clear policies must govern consultation recording practices. Patient consent must be documented before recording sessions. Recorded consultations require the same protection as other medical records.
2.3 Session security
Unique session identifiers prevent unauthorized access to consultations. Automatic session termination addresses abandoned connections. Waiting room controls prevent unauthorized users from joining sessions.
3. Data privacy regulations
Healthcare organizations operating across jurisdictions face multiple privacy regulations.
3.1 State telehealth laws
Each state has specific requirements for telehealth practice, consent, and prescribing. Interstate medical licensure compacts simplify multi-state practice. Platform design must accommodate varying state requirements.
3.2 International regulations
GDPR applies to European patient data, with specific consent and data-handling requirements. Other countries have emerging healthcare data regulations. International deployments require careful regulatory analysis.
4. Compliance documentation
Comprehensive documentation supports audit readiness and demonstrates a commitment to compliance.
4.1 Security policies
Document security policies covering access control, incident response, and data handling. Update policies regularly as regulations and best practices evolve. Train staff on policy requirements consistently.
4.2 Risk assessments
Conduct regular risk assessments as required by HIPAA. Document identified risks and mitigation measures. Track remediation efforts to completion.
4.3 Audit trails
Maintain comprehensive logs of system access and data handling. Retain logs for required periods, typically six years for HIPAA. Implement log analysis for security monitoring.
Common Telemedicine Development Challenges and Solutions
Healthcare technology projects face unique challenges that require experienced handling. Understanding common obstacles helps organizations prepare and address issues proactively.
Challenge 1: EHR integration complexity
Integrating with established EHR systems such as Epic and Cerner poses significant technical challenges. These systems use proprietary APIs and data formats that require specialized expertise.
Solution approach
Begin integration planning during the discovery phase to identify requirements early. Engage EHR vendors early to understand certification requirements and timelines. Use HL7 FHIR standards where possible to simplify data exchange. Our team has extensive experience with Epic EHR integration development and other major platforms.
Challenge 2: Video quality across network conditions
Patients connect from locations with varying internet quality. Poor video quality impacts clinical effectiveness and patient satisfaction.
Solution approach
Implement adaptive bitrate streaming that adjusts quality based on available bandwidth. Provide audio-only fallback options for patients with limited connectivity. Offer pre-consultation connectivity testing to proactively identify issues. Design interfaces that function effectively even during temporary video disruptions.
Challenge 3: Provider adoption resistance
Healthcare providers often resist new technology that changes established workflows. Low provider adoption undermines the success of telemedicine programs.
Solution approach
Involve providers in design decisions to ensure workflows meet clinical needs. Design interfaces that minimize documentation burden and click counts. Provide comprehensive training with hands-on practice opportunities. Identify physician champions who can promote adoption among peers.
Challenge 4: Patient technology barriers
Many patients, particularly older adults, face challenges with video consultation technology. Digital literacy gaps limit the reach of telemedicine programs.
Solution approach
Design simple, intuitive interfaces that minimize technology requirements. Offer multiple access options, including web, mobile, and phone-based consultations. Provide technical support resources for patients experiencing difficulties. Consider hardware programs that provide devices to patients lacking suitable equipment.
Challenge 5: Regulatory compliance across jurisdictions
Healthcare regulations vary significantly across states and countries. Multi-jurisdiction compliance creates substantial complexity.
Solution approach
Comprehensively map regulatory requirements during project planning. Build configurable compliance features that adapt to different requirements. Establish ongoing regulatory monitoring to identify changes in requirements. Partner with healthcare compliance experts for complex multi-jurisdiction deployments.
Challenge 6: Scalability under unexpected demand
Healthcare organizations experienced dramatic increases in telemedicine demand during recent health emergencies. Platforms must handle unexpected usage spikes.
Solution approach
Design a cloud-native architecture that scales automatically based on demand. Load test platforms at 3-5x expected peak capacity. Implement queue management features for high-demand periods. Plan capacity expansion procedures before they become necessary.
Addressing these complex development challenges requires specialized expertise and proven healthcare technology experience. Hire medical practice management software developers who understand the intricacies of regulatory compliance, secure architecture, and scalable infrastructure to build telemedicine platforms that deliver reliable, compliant, and patient-centered care at scale.
Partner with Space-O Technologies for Telemedicine Platform Development
Telemedicine platform development is transforming the way healthcare is delivered, offering greater access, efficiency, and patient engagement. From secure video consultations to integrated patient management, a well-designed telemedicine platform can redefine care delivery while ensuring compliance, scalability, and reliability.
At Space-O Technologies, we bring 15+ years of experience as a trusted software development partner with a specific focus on healthcare applications. With 300+ custom software solutions developed and 1200+ clients served, our team has the expertise to turn your telemedicine vision into a fully functional, secure, and scalable platform.
Our healthcare development credentials
We understand the unique requirements of healthcare technology projects.
- HIPAA compliance expertise built into every healthcare project.
- HL7 FHIR implementation experience for seamless interoperability.
- ISO 27001:2022 certification demonstrating security commitment.
- 98% client satisfaction rate verified through Upwork reviews.
- 140+ skilled developers, including healthcare specialists.
Featured telemedicine project: MedCall WorkComp
Our MedCall WorkComp case study demonstrates our telemedicine development capabilities.
- Project scope: Complete doctor-on-demand platform with patient apps, provider apps, and an administrative portal.
- Key features: Real-time video consultations, emergency triage workflows, prescription delivery, and multi-party video calls.
- Results achieved: The platform serves 20,000+ registered companies with 200+ active doctors. Delivered in 3 months from project kickoff to launch.
Whether you are a healthcare startup, hospital, or digital health company, our team can guide you through every step of telemedicine platform development, from feature planning and architecture design to deployment and ongoing support.
Ready to discuss your telemedicine platform project? Contact us for a consultation and project assessment.
FAQs on Telemedicine Platform Development
How long does it take to develop a telemedicine platform?
Development timelines depend on platform complexity and feature requirements. A basic telemedicine MVP typically takes 3–4 months to design, develop, and launch. Standard platforms with features such as appointment scheduling, EHR integration, and secure messaging usually require 5–8 months. Enterprise-grade telemedicine solutions with advanced capabilities like AI-driven diagnostics, multi-specialty workflows, and large-scale integrations may take 9–15 months or longer.
What does telemedicine platform development cost?
Telemedicine platform development costs vary based on feature scope, integrations, and technical complexity. A basic telemedicine MVP with core video consultation features typically costs between $40,000 and $75,000. Standard platforms that include scheduling, EHR integration, and e-prescribing generally range from $100,000 to $200,000. Enterprise solutions with advanced features, security layers, and extensive integrations start at $250,000 and can exceed $500,000.
Is HIPAA compliance required for all telemedicine platforms?
HIPAA compliance is required for telemedicine platforms that handle protected health information (PHI) for covered entities in the United States. This includes most healthcare providers, health plans, and their business associates. Even when HIPAA compliance is not legally mandatory, following HIPAA-level security practices helps protect patient data, builds trust, and prepares the platform for future regulatory and business growth.
Can telemedicine platforms integrate with existing EHR systems?
Yes, modern telemedicine platforms can integrate with leading EHR systems such as Epic, Cerner, and athenahealth. Successful integration requires familiarity with vendor-specific APIs, data models, and certification requirements. HL7 FHIR standards simplify this process by enabling standardized and secure data exchange between telemedicine platforms and EHR systems.
What technology stack works best for telemedicine development?
The ideal technology stack depends on your platform goals, scalability needs, and compliance requirements. React Native or Flutter are commonly used for cross-platform mobile app development. Node.js and Python are popular backend technologies for healthcare applications due to their flexibility and performance. PostgreSQL is widely used for secure, HIPAA-compliant data storage, while cloud providers such as AWS, Microsoft Azure, and Google Cloud offer healthcare-ready infrastructure and compliance support.
How do you ensure the quality and reliability of video consultations?
High-quality video consultations rely on both infrastructure and implementation best practices. WebRTC enables secure, real-time video communication directly in browsers without additional plugins. Commercial video APIs like Twilio and Agora provide HIPAA-compliant video services with global infrastructure support. Adaptive bitrate streaming helps maintain call quality under varying network conditions, while extensive testing across devices and network environments ensures consistent performance and reliability.