Contents
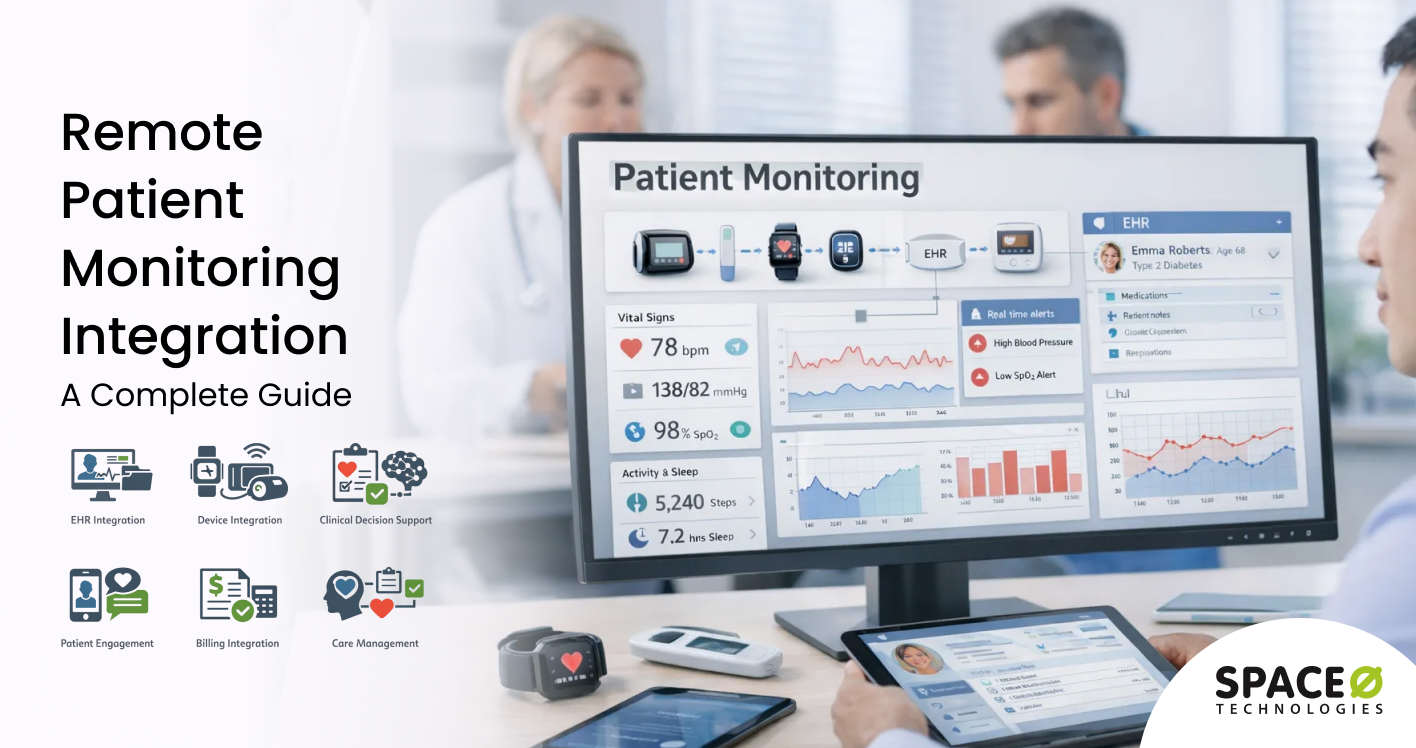
Remote patient monitoring software integration plays a critical role in delivering reliable and connected digital care experiences. An RPM platform must seamlessly integrate with medical devices, wearables, EHR systems, analytics tools, and care management workflows to deliver accurate, real-time patient insights.
As RPM ecosystems grow more complex, integration challenges often become the biggest barrier to scalability and clinical adoption. Disconnected systems, inconsistent data formats, and unreliable device connectivity can compromise data accuracy, clinician trust, and patient safety.
This guide covers everything you need to know about remote patient monitoring software integration. Drawing from 15+ years of experience as a trusted remote patient software development company, we have shared insights on integration fundamentals, common integration approaches, implementation process, cost considerations, key challenges, and best practices for building secure and scalable RPM integrations.
What is Remote Patient Monitoring Integration?
Remote patient monitoring integration refers to connecting RPM devices, applications, and data platforms with healthcare IT infrastructure, including EHR systems, clinical workflows, billing systems, and patient engagement tools. These integrations enable automatic transmission of patient health data from monitoring devices to clinical systems where providers can review, analyze, and act on the information.
Modern RPM integration relies on healthcare interoperability standards such as HL7 FHIR (Fast Healthcare Interoperability Resources) and APIs that enable different systems to exchange data in standardized formats. When a patient measures their blood pressure at home using a connected device, integration automatically transmits the reading to their electronic health record, triggers alerts if values exceed thresholds, and updates care management dashboards.
Healthcare system integration has become essential as organizations deploy multiple RPM solutions for different conditions. A single health system may use separate devices for blood glucose monitoring, cardiac monitoring, pulse oximetry, and weight management. Without integration, each data stream remains isolated, requiring clinicians to access multiple systems and manually correlate information.
Benefits of Remote Patient Monitoring Integration
Integrating your remote patient monitoring systems delivers measurable improvements across clinical care, operational efficiency, and financial performance. These benefits compound as connected systems enable more sophisticated care models.
1. Create a unified patient health record
Integration consolidates RPM data with clinical documentation in the EHR, creating a comprehensive patient health record. Providers see vital signs, symptoms, and trends alongside medical history, medications, and lab results. This complete visibility improves clinical decision-making and care coordination.
2. Enable real-time clinical alerts and interventions
Connected RPM systems deliver alerts directly into clinical workflows when patient data exceeds defined thresholds. Instead of reviewing data hours or days later, care teams receive immediate notifications, enabling timely interventions. Early detection of deterioration reduces emergency department visits and hospitalizations.
3. Reduce manual data entry and transcription errors
Automated data transmission eliminates the need for staff to manually enter RPM readings into clinical systems. This automation reduces transcription errors that can lead to incorrect clinical decisions and recovers significant time previously spent on data entry tasks.
4. Support chronic care management reimbursement
Integrated RPM data documentation supports billing for chronic care management (CCM) and remote physiologic monitoring CPT codes. When monitoring data flows automatically into clinical records with timestamps and provider review documentation, organizations capture revenue from CPT codes 99453-99458 more reliably.
5. Improve patient engagement and adherence
Integration enables bidirectional communication between patients and care teams through connected portals and messaging systems. Patients receive personalized feedback based on their monitoring data, improving engagement with care plans and adherence to monitoring schedules.
6. Enable population health analytics
Aggregated RPM data from integrated systems powers population health analytics and risk stratification. Organizations identify high-risk patients who require proactive outreach, measure the effectiveness of interventions, and demonstrate quality outcomes for value-based contracts.
7. Streamline clinical workflows and reduce alert fatigue
Well-designed integration delivers actionable information within existing clinical workflows rather than creating separate monitoring burdens. Smart filtering and escalation rules ensure clinicians see meaningful alerts without drowning in notifications.
Need Help Integrating Your RPM Systems?
Connect your remote patient monitoring devices and platforms with expert integration services from Space-O Technologies. We build secure, HIPAA-compliant integrations using HL7 FHIR standards that streamline your clinical workflows.

Essential Remote Patient Monitoring Integrations
Not all integrations deliver equal clinical and operational value. Prioritize connections that directly impact patient care, workflow efficiency, and revenue capture. These essential integrations form the foundation of effective RPM programs.
1. RPM EHR integration
Electronic health record integration represents the most critical connection for remote patient monitoring programs. This integration synchronizes patient demographics, device data, vital signs, and clinical documentation between RPM platforms and EHR systems.
Key capabilities
- Automatic transmission of device readings to patient charts
- Bidirectional patient demographic synchronization
- Clinical alert routing to appropriate care team members
- Documentation templates for RPM review and interventions
- Trending and visualization of monitoring data within EHR
Impact: Healthcare organizations with tight RPM-EHR integration report faster clinical response to abnormal readings and improvement in care plan adherence documentation.
2. Medical device and wearable integration
Connecting diverse monitoring devices to your RPM platform requires standardized approaches to handle different manufacturers, data formats, and transmission protocols.
Key capabilities
- Support for Bluetooth, cellular, and WiFi device connectivity
- Standardized data normalization across device manufacturers
- Device provisioning and remote configuration management
- Battery and connectivity status monitoring
Impact: Standardized device integration enables organizations to select best-of-breed monitoring equipment without platform lock-in.
3. Clinical decision support integration
Integrating RPM data with clinical decision support (CDS) tools enables automated analysis and recommendations based on monitoring trends.
Key capabilities
- Rule-based alerting with configurable thresholds
- Trend analysis identifying gradual deterioration patterns
- Risk scoring incorporating RPM data with other clinical factors
- Predictive analytics for early intervention opportunities
Impact: CDS integration transforms raw monitoring data into actionable clinical intelligence, enabling proactive care management.
4. Patient portal and engagement integration
Patient-facing tools must connect with RPM systems to enable self-service features and bidirectional communication.
Key capabilities
- Patient access to their own monitoring data and trends
- Secure messaging between patients and care teams
- Educational content delivery based on monitoring results
- Appointment scheduling triggered by monitoring events
Impact: Integrated patient engagement tools improve monitoring adherence and reduce unnecessary office visits through virtual check-ins.
5. Billing and revenue cycle integration
Connecting RPM documentation with billing systems ensures accurate capture of reimbursable services and streamlines claims submission.
Key capabilities
- Automatic documentation of time spent reviewing RPM data
- CPT code suggestion based on services provided
- Claims generation with supporting documentation
- Eligibility verification for RPM coverage
Impact: Automated billing integration reduces revenue leakage from undocumented RPM services and accelerates reimbursement cycles.
6. Care management platform integration
For organizations using dedicated care management software, integration ensures RPM data informs care coordination activities.
Key capabilities
- Care plan updates based on monitoring outcomes
- Task assignment triggered by RPM alerts
- Population health dashboards incorporating RPM metrics
- Quality measure reporting with RPM data elements
Impact: Care management integration enables RPM programs to scale efficiently while maintaining personalized patient engagement.
Looking to Connect Your RPM Devices with EHR Systems?
Work with Space-O Technologies to build custom RPM integrations using HL7 FHIR standards. Our healthcare software development team has 15+ years of experience building HIPAA-compliant interoperability solutions.
Types of Remote Patient Monitoring Integration Approaches
Different integration methods suit different scenarios based on existing infrastructure, technical capabilities, and organizational requirements. Understanding these approaches helps you select the right strategy.
| Approach | Best For | Complexity | Flexibility | Maintenance |
|---|---|---|---|---|
| Native EHR Modules | Connecting RPM features within the existing EHR | Low | Limited to EHR vendor offerings | Vendor managed |
| HL7 FHIR APIs | Standards-based healthcare data exchange | Medium | Highly standardized approach | Industry standard updates |
| SMART on FHIR | Embedding RPM apps within EHR workflows | Medium | App-based flexibility | App + platform updates |
| Integration Engines | Connecting multiple systems with data transformation | Medium-High | Pre-built connectors available | Platform subscription + configuration |
| Custom API Development | Proprietary systems or unique requirements | High | Unlimited flexibility | Significant ongoing maintenance |
1. Native EHR integration modules
Major EHR vendors, including Epic, Cerner, and Athenahealth, offer built-in RPM modules or app marketplace integrations. These native connections provide tested compatibility within the EHR ecosystem.
- Advantages: Pre-validated integration reduces implementation risk. Updates managed by the EHR vendor. Tight workflow integration within familiar clinical interfaces.
- Limitations: Limited to devices and features supported by the EHR vendor. May not support specialized monitoring requirements.
2. HL7 FHIR API integration
HL7 FHIR has become the modern standard for healthcare data exchange, leveraging familiar web technologies such as REST and JSON. FHIR provides standardized resource definitions for patient data, observations, and clinical documents.
- Advantages: Industry-standard support from major EHR vendors. Regulatory compliance with 21st Century Cures Act requirements.
- Limitations: FHIR implementation varies across vendors despite standardization. Complex clinical scenarios may require custom FHIR profiles.
3. SMART on FHIR integration
SMART on FHIR enables RPM applications to launch within EHR workflows while accessing patient data through FHIR APIs. This approach embeds monitoring tools directly in clinical workflows.
- Advantages: Seamless user experience within the EHR interface. Standardized authorization and authentication.
- Limitations: Requires EHR support for SMART on FHIR. Application development must follow SMART specifications.
4. Healthcare integration engines
Integration engines such as MuleSoft, Rhapsody, and InterSystems HealthShare provide middleware platforms for connecting healthcare applications and enabling data transformation.
- Advantages: Centralizes integration management across multiple systems. Handles protocol and format translation.
- Limitations: Platform licensing and infrastructure costs. Requires specialized integration expertise.
5. Custom API development
For unique requirements or proprietary systems without standard interfaces, custom API development enables tailored integration solutions.
- Advantages: Addresses specific organizational requirements. Full control over integration behavior.
- Limitations: Higher development and maintenance costs. Requires ongoing support as systems change.
Key Integration Standards for Remote Patient Monitoring
When you outsource remote patient monitoring software, RPM integration requires understanding healthcare interoperability standards that govern data exchange. These standards ensure consistent, secure, and compliant data transmission.
1. HL7 FHIR (Fast Healthcare Interoperability Resources)
FHIR represents the current standard for healthcare API development. It defines resources for clinical data, including Observations (vital signs), Patients, Devices, and CarePlans relevant to RPM. FHIR R4 is the current production standard, with implementation guides like US Core defining specific requirements for US healthcare.
2. HL7 Version 2.x messaging
HL7 v2 remains widely deployed for traditional healthcare messaging, particularly for ADT events and results delivery. Many organizations maintain HL7 v2 alongside FHIR adoption for legacy system compatibility.
3. IEEE 11073 Personal Health Device Standards
IEEE 11073 defines communication standards for personal health devices, enabling plug-and-play interoperability between RPM devices and aggregating platforms. Device manufacturers increasingly support IEEE 11073 for Bluetooth communication with blood pressure monitors, pulse oximeters, weight scales, and glucose meters.
4. Continua Design Guidelines
The Continua Design Guidelines extend IEEE 11073 with end-to-end interoperability specifications from device to EHR. Continua certification indicates tested interoperability and addresses security, transport, and data format requirements.
Common Challenges in Remote Patient Monitoring Integration
Even well-planned RPM integration projects encounter obstacles. Anticipating these challenges enables proactive solutions.
Challenge 1: Data fragmentation across multiple device vendors
Different RPM device manufacturers use varying data formats, transmission protocols, and measurement standards.
How to overcome this challenge
- Implement a device-agnostic aggregation layer that normalizes data formats
- Require vendor support for IEEE 11073 or FHIR device standards in procurement
- Create comprehensive data mapping specifications for each device type
- Build validation rules to catch data quality issues before clinical use
Challenge 2: EHR vendor API limitations and costs
Major EHR vendors may limit API access, charge significant integration fees, or provide insufficient documentation.
How to overcome this challenge
- Engage EHR vendors early in integration planning to understand capabilities and costs
- Leverage the 21st Century Cures Act requirements for patient access APIs
- Explore EHR marketplace applications as an alternative to custom integration
- Negotiate API access terms as part of EHR contract renewals
Challenge 3: Clinical workflow disruption
Integrations that interrupt clinical workflows or create additional burden face provider resistance regardless of technical success.
How to overcome this challenge
- Involve clinical end users in integration design from the beginning
- Map current workflows before designing integration touchpoints
- Implement smart alerting with appropriate thresholds to prevent alert fatigue
- Provide training and change management support for new workflows
Challenge 4: HIPAA compliance and data security
RPM integration creates data transmission pathways that must protect patient health information throughout the exchange process.
How to overcome this challenge
- Encrypt all data in transit using TLS 1.2 or higher
- Implement OAuth 2.0 authentication for API access
- Conduct security risk assessments for all integration points
- Include Business Associate Agreements with all integration partners
Challenge 5: Scalability and performance under load
Integration architectures that work for pilot programs may struggle when scaled to enterprise RPM deployments.
How to overcome this challenge
- Load test integrations with realistic data volumes before production
- Design message queuing for high-volume data streams
- Implement horizontal scaling capabilities from the beginning
- Monitor integration performance continuously with alerting for degradation
Challenge 6: Maintaining integrations across system updates
EHR upgrades, device firmware changes, and API version updates can break existing integrations.
How to overcome this challenge
- Establish change notification processes with all integration partners
- Maintain staging environments that mirror production for testing updates
- Document all integration configurations and dependencies
- Build automated testing to validate the integration function after changes
Get Expert RPM Integration Support From Space-O Technologies
Work with Space-O Technologies to build secure, scalable remote patient monitoring integrations tailored to your clinical workflows. Our team has delivered 300+ healthcare software solutions.
Best Practices for Successful RPM Integration
Following proven practices dramatically increases integration success rates. Implement these guidelines from project inception.
1. Start with clinical requirements, not technical specifications
Document the clinical problems integration should solve before diving into technical architecture. Understand what information clinicians need, when they need it, and how they want to receive it. Engage physicians, nurses, and care managers in defining integration requirements.
2. Adopt standards-based integration wherever possible
Prioritize HL7 FHIR and other healthcare interoperability standards over proprietary interfaces. Standards-based integration reduces long-term maintenance burden, improves vendor flexibility, and positions your organization for regulatory compliance.
3. Design for bidirectional data flow
Effective RPM integration enables bidirectional data flow. Patient data flows from devices to clinical systems, while care instructions and feedback flow back to patients. Design an integration architecture to support bidirectional communication from the start.
4. Implement comprehensive error handling and monitoring
Build robust error handling that captures, logs, and alerts on integration failures. Create dashboards that visualize integration health, including message volumes, latency, and error rates. Silent integration failures can result in missed clinical alerts with patient safety implications.
5. Plan for device diversity and evolution
RPM technology evolves rapidly. Design an integration architecture that accommodates new devices, updated protocols, and emerging standards without major rearchitecture. A device-agnostic approach enables flexibility in selecting devices and adopting technologies.
6. Test thoroughly with realistic clinical scenarios
Create test cases that mirror actual clinical workflows, including edge cases and failure scenarios. Test with realistic data volumes and involve clinical users in user acceptance testing to validate workflow integration.
7. Document everything for operational sustainability
Create comprehensive documentation covering integration architecture, configuration, data mappings, and troubleshooting procedures. Keep documentation up to date as integrations evolve for future team members and support staff.
Hire Our Integration Experts to Connect Your RPM Systems with Clinical Workflows
Remote patient monitoring integration transforms isolated device data into actionable clinical intelligence within care team workflows. The right integrations reduce administrative burden, enable real-time interventions, improve patient outcomes, and support sustainable economics for RPM programs. Organizations that master RPM integration deliver better care while capturing appropriate reimbursement.
Success requires understanding healthcare interoperability standards, navigating EHR vendor relationships, and designing integrations that support clinical workflows rather than disrupt them. Integration is not simply a technical project but a clinical transformation that affects how care teams interact with monitoring data.
Space-O Technologies specializes in healthcare software development services with expertise in remote patient monitoring and patient portal development. Our team has built platforms that connect RPM devices to major EHR systems, including Epic and Cerner, using HL7 FHIR standards. We understand the technical requirements and regulatory considerations that make healthcare integration challenging.
With 15+ years of experience, 300+ software solutions delivered, and ISO 27001 certification for information security, we bring proven capabilities to your integration project. Our software development consulting services help you plan integration strategies while our development teams execute with precision.
Contact us today to discuss your remote patient monitoring integration requirements and discover how connected systems can enhance your RPM program outcomes.
FAQs on Remote Patient Monitoring Integration
1. What is RPM EHR integration, and why is it important?
RPM EHR integration connects remote patient monitoring devices with electronic health record systems, enabling automatic transmission of patient vital signs into clinical records. This integration eliminates manual data entry, ensures complete and accurate patient records, enables real-time clinical alerts, and supports documentation required for RPM reimbursement programs.
2. Which EHR systems support remote patient monitoring integration?
Most major EHR systems support remote patient monitoring integration, including Epic, Cerner (Oracle Health), Athenahealth, and Allscripts. Epic enables integration through its App Orchard marketplace and FHIR APIs. In addition, most modern EHR platforms support HL7 FHIR APIs as mandated by the 21st Century Cures Act, allowing standardized RPM data exchange.
3. What is HL7 FHIR, and how does it apply to RPM integration?
HL7 FHIR (Fast Healthcare Interoperability Resources) is a modern standard for healthcare data exchange. It defines structured resources for vital signs, medical devices, and patient demographics. In RPM integration, FHIR enables standardized transmission of monitoring data into EHRs and serves as the foundation for SMART on FHIR applications that embed RPM insights directly into clinical workflows.
4. How do you integrate wearable devices with healthcare systems?
Wearable device integration involves multiple layers. Devices transmit data via Bluetooth to mobile apps or hub devices, which then send data to cloud platforms for normalization and clinical rule processing. The normalized data is transmitted to EHR systems via APIs. Standards such as IEEE 11073 support device-to-platform interoperability, while HL7 FHIR enables platform-to-EHR integration.
5. What security measures are required for RPM integration?
RPM integration must protect patient health information during transmission and storage. Key security measures include encryption for data in transit (TLS 1.2 or higher), secure authentication using OAuth 2.0, role-based access controls, detailed audit logging, and Business Associate Agreements (BAAs) with integration partners. All components of RPM integration must comply with HIPAA requirements.
6. How long does RPM integration typically take to implement?
RPM integration timelines depend on complexity and scope. Simple integrations using vendor-supported connectors typically take 4–8 weeks. Custom integrations with major EHR systems generally require 8–16 weeks, including design, development, testing, and go-live support. Complex multi-system integrations may take 16–24 weeks, depending on EHR vendor coordination and clinical workflow requirements.
7. What is the difference between device integration and EHR integration for RPM?
Device integration focuses on connecting monitoring equipment such as blood pressure cuffs, pulse oximeters, and weight scales to RPM platforms, managing data transmission and normalization. EHR integration connects RPM platforms with clinical systems, enabling monitoring data to flow into patient records and clinical workflows. A complete RPM solution requires both layers to work together seamlessly.