Contents
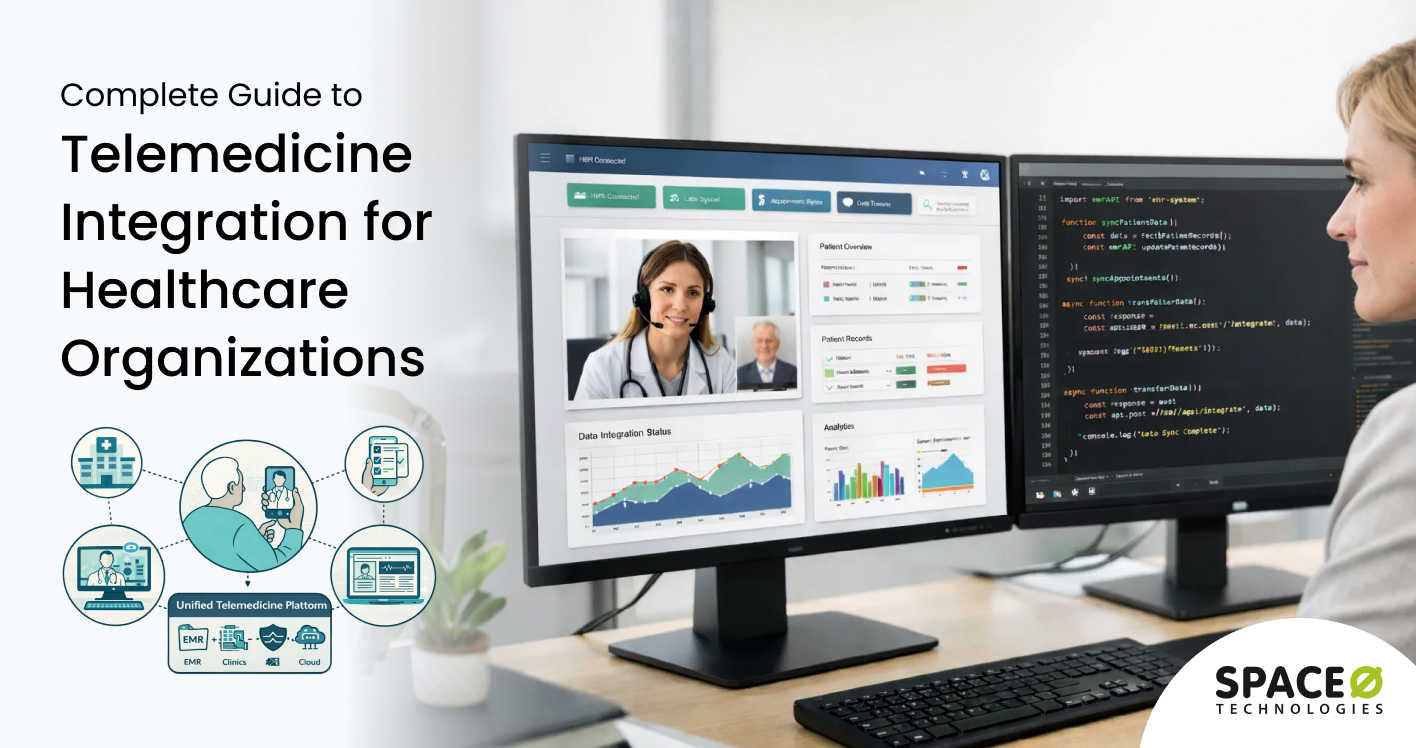
Telemedicine platforms deliver real value only when they work seamlessly with existing healthcare systems. Video consultations alone are not enough. To support efficient care delivery, telemedicine solutions must integrate with electronic health records, scheduling systems, billing platforms, diagnostic tools, and patient communication channels.
Telemedicine integration ensures that data flows securely and accurately across systems without manual intervention. It enables clinicians to access patient records in real time, automate workflows, reduce administrative burden, and maintain continuity of care across digital and in-person touchpoints. Poor integration, on the other hand, leads to data silos, workflow disruptions, and compliance risks that can be addressed through custom telemedicine software development services.
This blog explains what telemedicine integration involves, the systems commonly integrated with telemedicine platforms, key challenges to consider, and best practices for successful implementation. Drawing from our experience as a leading telemedicine development company, we’ve shared insights to help you plan integrations that support long-term scalability and operational efficiency.
What is Telemedicine Integration?
Telemedicine integration refers to connecting virtual care platforms with other healthcare information systems. It enables seamless data flow between telehealth applications and EHRs, practice management systems, and billing platforms. This connectivity creates unified workflows in which patient information is automatically moved between systems.
The core goal is to eliminate data silos that fragment patient care. When systems integrate properly, clinicians access complete patient histories during virtual consultations. They document visits directly into EHRs without switching applications. Lab results, prescriptions, and referrals flow automatically to the appropriate destinations.
Modern telemedicine integration relies on standardized protocols and APIs to exchange healthcare data. These technical standards ensure that different vendor systems communicate effectively. Organizations can connect best-of-breed solutions rather than accepting single-vendor limitations.
Key components of telemedicine integration
Successful telemedicine integration requires multiple technical and operational components working together. Each element plays a critical role in creating seamless clinical workflows.
- Data exchange protocols form the foundation of healthcare interoperability. Standards like HL7 FHIR define how systems structure and transmit patient information. These protocols ensure consistent data formatting across diverse applications.
- API connections enable real-time communication between telemedicine platforms and external systems. RESTful APIs allow applications to request and share information on demand. Well-designed APIs handle authentication, data validation, and error management automatically.
- Clinical workflow mapping aligns technical integrations with actual care delivery processes. Integration designs must support how clinicians actually work during consultations. Poor workflow alignment leads to workarounds that undermine the benefits of integration.
- Security infrastructure protects sensitive patient data throughout transmission and storage. HIPAA compliance requires encryption, access controls, and audit logging for all integration points. Security cannot be retrofitted after integration deployment.
Why Healthcare Organizations Need Telemedicine Integration
The business case for telemedicine integration extends beyond patient satisfaction alone. Operational efficiency improvements reduce costs while enabling higher patient volumes. Partnering with the best telemedicine software development firms ensures clinicians spend more time on care delivery and less time on administrative tasks.
1. Clinical benefits of connected telehealth systems
Integrated telemedicine platforms directly improve care quality and patient safety. Clinicians make better decisions when they have complete patient information at their disposal.
Access to comprehensive medical histories during virtual visits prevents medication errors and missed diagnoses. Providers see allergies, current prescriptions, and recent test results without hunting through separate systems. This complete picture enables informed, real-time clinical decision-making.
Continuity of care improves when telehealth documentation flows automatically into patient records. Future providers see virtual visit notes alongside in-person encounters. Nothing falls through the cracks between care settings.
Care coordination becomes practical when referring providers receive consultation notes automatically. Specialists document recommendations that primary care physicians can access immediately. Patients experience smoother transitions between providers and care settings.
2. Operational advantages of telehealth integration
Beyond clinical improvements, integration delivers measurable operational benefits to healthcare organizations. Administrative burden decreases while revenue capture increases.
Staff productivity increases when manual data entry disappears from clinical workflows. Medical assistants no longer transcribe information between systems. Clinicians document once and trust that data propagates appropriately.
Billing accuracy improves when charge capture connects directly to clinical documentation. Procedure codes are automatically linked to diagnosis codes in the encounter record. Fewer claims require manual review before submission.
Scheduling optimization becomes possible when appointment systems connect to clinical and billing data. Organizations identify utilization patterns and patient preferences across channels. Capacity planning incorporates both virtual and in-person demand.
3. Patient experience improvements
Patients increasingly expect digital healthcare experiences that match other industries. Fragmented systems create friction that undermines satisfaction and retention.
Pre-visit paperwork decreases when intake forms populate from existing patient records. Patients confirm information rather than re-entering demographics, insurance, and medical history. Registration takes minutes instead of requiring lengthy questionnaires.
Post-visit access improves when patient portals display telehealth encounters alongside other records. Patients review visit summaries, access prescriptions, and message providers through familiar interfaces. They avoid juggling multiple apps and logins.
Prescription fulfillment accelerates when e-prescribing connects directly to pharmacy networks. Providers transmit prescriptions during virtual visits without manual steps. Patients pick up medications or receive home delivery without delays.
Need Expert Telemedicine Integration Support?
Space-O Technologies builds integrated telemedicine solutions that connect seamlessly with EHR systems, billing platforms, and clinical workflows.

Key Platforms To Integrate Into Your Telemedicine Solution
Healthcare organizations pursue different integration approaches based on their existing technology landscape. Understanding these categories helps leaders select appropriate strategies for their specific situations.
1. EHR and EMR integration
Electronic health record integration represents the most critical connection for telemedicine platforms. EHR integration enables bidirectional data flow between virtual care tools and core clinical systems.
- Epic EHR integration connects telemedicine platforms with the most widely deployed hospital system. Epic serves over 250 million patients through its customer base. Integration typically uses Epic’s App Orchard marketplace and FHIR APIs.
- Cerner integration links telehealth tools with another dominant hospital EHR platform. Oracle Cerner provides clinical systems to thousands of healthcare facilities. Their Millennium platform offers multiple integration pathways, including FHIR.
- Athenahealth integration connects cloud-based ambulatory EHR with telemedicine capabilities. The athenaOne platform serves primarily outpatient practices and clinics. Their API marketplace simplifies third-party application connectivity.
- AllScripts integration enables telehealth connectivity with their suite of clinical products. Practices using Sunrise Clinical Manager or Professional EHR benefit from documented integration specifications.
2. Practice management system integration
Beyond EHRs, telemedicine platforms must integrate with systems for appointment scheduling, billing, and administrative workflows. Practice management integration streamlines operations across the revenue cycle.
- Scheduling system integration synchronizes appointment availability across virtual and in-person channels. Patients book telehealth visits through existing scheduling interfaces. Providers manage unified calendars without switching between applications.
- Billing system integration ensures telehealth encounters generate appropriate claims automatically. Charge capture connects to payer requirements and fee schedules. Revenue integrity improves through automated verification processes.
- Patient registration integration shares demographic and insurance information across platforms. Staff avoid entering patient details multiple times. Data quality improves when single sources of truth propagate throughout the system.
3. Third-party clinical integration
Telemedicine platforms frequently connect with specialized clinical systems beyond core EHRs. These integrations expand platform capabilities and support comprehensive care delivery.
- E-prescribing integration transmits medication orders directly to pharmacies during virtual visits. Surescripts network connectivity enables prescription routing to 99% of U.S. pharmacies. Controlled substance prescribing requires EPCS-certified integrations.
- Lab system integration enables ordering diagnostic tests during telehealth encounters. Results return automatically to ordering providers for review. Patients avoid unnecessary follow-up visits for routine result discussions.
- Remote patient monitoring integration brings device data into telemedicine workflows. Blood pressure cuffs, glucose monitors, and wearables continuously transmit readings. Providers review trends during virtual consultations.
- Imaging integration incorporates radiology and diagnostic images into virtual encounters. DICOM standards enable viewing of X-rays, MRIs, and CT scans. Store-and-forward telehealth benefits particularly from imaging connectivity.
4. Payment and insurance integration
Financial integrations ensure telemedicine services generate appropriate revenue while minimizing patient friction. Payment processing connects the clinical encounter to revenue capture.
- Payment gateway integration enables patient copay collection during or after virtual visits. Stripe, Square, and healthcare-specific processors handle transaction security. Patients appreciate convenient payment options that match other digital experiences.
- Insurance verification integration confirms coverage before appointments begin. Real-time eligibility checks prevent surprise billing situations. Staff spend less time on manual verification phone calls.
- Claims submission integration routes encounters to the appropriate payers automatically. Clearinghouse connections handle formatting and transmission requirements. Denial rates decrease through automated validation before submission.
Healthcare Integration Standards and Protocols
Successful telemedicine integration depends on adopting appropriate technical standards. These protocols ensure consistent data exchange across diverse healthcare systems. Understanding available standards helps organizations make informed integration decisions.
1. HL7 FHIR standard
Fast Healthcare Interoperability Resources has become the dominant healthcare data exchange standard. FHIR combines modern web technologies with healthcare-specific data models. According to a 2024 HIMSS report, 78% of healthcare providers using HL7 FHIR experienced faster care coordination.
FHIR uses RESTful API patterns familiar to modern software developers. Resources represent clinical concepts like patients, observations, and medications. JSON and XML formatting options support diverse implementation preferences.
SMART on FHIR extends the base standard with authorization and application launch capabilities. This specification enables third-party apps to securely integrate with EHRs. Users launch applications directly from within their clinical systems.
Adoption continues accelerating as regulations mandate FHIR support. CMS and ONC rules require FHIR APIs for certified health IT products. Now, 84% of hospitals use FHIR APIs for at least some data exchange.
2. HL7 v2 messaging
Despite FHIR’s growth, HL7 Version 2 remains widely deployed in healthcare organizations. This older standard handles common transactions like admissions, orders, and results. Many legacy systems support only v2 messaging.
ADT messages communicate patient admission, discharge, and transfer events. These transactions automatically trigger workflows across connected systems. Real-time ADT feeds keep patient census up to date across the entire system.
ORM and ORU messages handle orders and results, respectively. Lab systems receive order requests and return completed results. These message types form the backbone of diagnostic workflows.
Organizations integrating with older systems often need v2 support alongside FHIR. Translation layers convert between standards when direct communication fails. Hybrid approaches balance legacy support with modernization goals.
3. CDA documents
Clinical Document Architecture provides standards for the exchange of clinical documents. CDA documents package narrative text with structured data elements. Common document types include discharge summaries and continuity-of-care documents.
C-CDA represents the consolidated implementation guide for U.S. healthcare. Meaningful Use regulations drove widespread adoption of C-CDA across EHR vendors. Patient summaries typically use C-CDA formatting for portability.
While CDA enables document sharing, FHIR increasingly handles discrete data exchange needs. Modern integrations often appropriately combine both approaches. Documents are well-suited for summary information, while APIs handle real-time transactions.
4. DICOM for imaging
Digital Imaging and Communications in Medicine standardizes medical image exchange. Radiology, cardiology, and other imaging specialties rely on DICOM formats. Telemedicine platforms incorporating images need DICOM viewer capabilities.
DICOM handles both image files and associated metadata comprehensively. Patient demographics, study information, and acquisition parameters travel with images. Receiving systems display images with full clinical context.
Teleradiology applications depend heavily on DICOM integration capabilities. Remote radiologists receive studies, perform interpretations, and return reports electronically. DICOM infrastructure enables distributed reading workflows.
Need HL7 FHIR Integration Expertise?
Our healthcare developers implement FHIR-compliant integrations connecting telemedicine platforms with Epic, Cerner, athenahealth, and other major EHR systems. We help you achieve interoperability faster.
Essential Telemedicine Integration Capabilities
Effective telemedicine integration requires specific capabilities that support clinical workflows. These features transform basic connectivity into meaningful interoperability. Organizations should prioritize these capabilities when planning integration projects.
1. Real-time data synchronization
Bidirectional synchronization keeps information continuously up to date across connected systems. Changes made anywhere propagate immediately to relevant destinations. Clinicians always see the latest patient information regardless of source.
Patient demographic updates flow automatically between registration systems and clinical applications. Address changes, insurance updates, and contact information are kept in sync. Staff avoid discrepancies that create billing and communication problems.
Clinical documentation synchronizes as providers complete notes and orders. Visit summaries appear in patient portals shortly after the encounter concludes. Referring providers can access consultation notes without waiting for faxes.
Appointment status changes are reflected immediately across scheduling interfaces. Cancellations and reschedules update availability for other patients. No-show tracking informs outreach and waitlist management workflows.
2. Single sign-on authentication
SSO eliminates multiple login requirements for clinicians accessing integrated systems. One authentication provides access to the telemedicine platform, EHR, and connected applications. Provider efficiency improves dramatically when password barriers disappear.
OAuth 2.0 protocols handle secure authorization between applications. Users authenticate once and receive tokens granting appropriate access. Security improves because fewer password entries reduce phishing risks.
Identity federation connects organizational directories with clinical applications. Active Directory or similar systems serve as authoritative identity sources. User provisioning and deprovisioning happen centrally with automatic propagation.
Role-based access controls ensure users see appropriate information everywhere. Administrative staff can access scheduling without exposing clinical data. Providers see complete records, while support staff see limited views.
3. Automated clinical workflows
Integration enables automated workflows that reduce manual intervention. Triggered actions execute automatically when defined conditions are met. Staff focus on exceptions rather than routine transactions.
Order routing delivers requests to appropriate destinations without manual intervention. Lab orders are automatically entered into laboratory information systems. Pharmacy orders are transmitted directly to the patient’s preferred pharmacies.
Result notification alerts providers when critical values require immediate attention. Abnormal findings trigger messages through preferred communication channels. Nothing falls through the cracks between the availability of results and provider awareness.
Referral management automatically tracks consultation requests through completion. Sending providers receive updates as specialists accept and complete referrals. Patients get appointments scheduled without playing phone tag.
4. Comprehensive audit logging
HIPAA compliance requires detailed tracking of access to protected health information. Integrated systems must log who accessed what information and when. Audit trails support compliance reporting and incident investigation.
Access logs capture user identities, timestamps, and specific records viewed. Unusual access patterns trigger security review alerts. Investigation tools help quickly identify inappropriate access.
Transaction logs track data exchanges between integrated systems. Organizations verify that information is transmitted correctly and completely. Troubleshooting integration issues becomes possible with detailed logs.
Consent management tracks patient authorizations for information sharing. Some patients restrict data disclosure beyond immediate care needs. Systems automatically enforce these preferences across integration points.
Telemedicine Integration Implementation Process
Successful integration projects follow structured implementation approaches. This process framework guides organizations from planning through optimization. Each phase builds a foundation for subsequent stages.
Phase 1: Discovery and requirements (4 to 8 weeks)
The discovery phase establishes integration scope and technical requirements. Stakeholders align on priorities while technical teams assess feasibility.
Key activities:
- Document current workflows and pain points through stakeholder interviews.
- Inventory source and target systems, including versions and interface capabilities.
- Define integration requirements in detailed specifications with acceptance criteria.
- Assess security and compliance requirements affecting design decisions.
- Develop preliminary architecture and integration patterns.
- Create a project plan with milestones, resources, and a budget.
Phase 2: Design and development (8 to 16 weeks)
Development transforms requirements into working integration components. Iterative approaches enable early feedback and course correction. At this stage, you can partner with a healthcare software development company like Space-O Technologies and get expert support for telemedicine platform integration.
Key activities:
- Design a detailed integration architecture, including data mappings and workflows.
- Develop integration components using appropriate standards and tools.
- Build unit tests validating individual component behavior.
- Create integration tests exercising end-to-end data flows.
- Document APIs and data specifications for ongoing maintenance.
- Conduct code review, ensuring quality and security compliance.
Phase 3: Testing and validation (4 to 8 weeks)
Comprehensive testing validates integration readiness for production deployment. Multiple testing types ensure thorough coverage.
Key activities:
- Execute functional testing to verify that requirements are satisfied.
- Perform integration testing with connected systems in the staging environment.
- Conduct performance testing under realistic load conditions.
- Complete security testing, including penetration testing of integration endpoints.
- Run user acceptance testing with clinical and operational stakeholders.
- Remediate defects identified during testing cycles.
Phase 4: Deployment and go-live (2 to 4 weeks)
Deployment transitions integration from testing into production operation. Careful planning minimizes disruption to clinical operations.
Key activities:
- Execute the deployment runbook in the production environment.
- Validate integration functionality with production data flows.
- Monitor system performance and error rates closely.
- Provide hypercare support during the initial operation period.
- Address issues identified during early production operation.
- Conduct a go-live review documenting lessons learned.
Phase 5: Optimization and expansion (ongoing)
Post-deployment optimization maximizes integration value while supporting evolution. Continuous improvement drives ongoing benefits.
Key activities:
- Monitor integration performance metrics and availability.
- Implement enhancements based on user feedback and new requirements.
- Manage vendor system upgrades affecting integrations.
- Expand integration scope to additional systems and workflows.
- Conduct periodic security assessments and compliance reviews.
- Update the documentation to reflect the current integration state.
Integrate Your Telemedicine Platform with Legacy Systems with Expert Guidance
Talk to Space-O Technologies to plan and implement seamless telemedicine integrations for your healthcare platform
Telemedicine Integration Challenges and Solutions
Healthcare integration projects encounter predictable obstacles that derail timelines and budgets. Understanding common challenges enables proactive mitigation strategies. Experienced teams anticipate these issues and plan accordingly.
Challenge 1: Legacy system compatibility
Many healthcare organizations run clinical systems designed before modern integration standards. These legacy platforms lack APIs and support only proprietary interfaces. Connecting telehealth tools requires creative technical approaches.
How to overcome this challenge
- Deploy integration engines that translate between modern APIs and legacy formats automatically.
- Implement HL7 v2 interfaces when FHIR APIs are unavailable on older systems.
- Consider middleware solutions that bridge incompatible systems through standardized connections.
- Plan phased modernization that replaces legacy systems incrementally while maintaining integration.
- Document legacy interface specifications thoroughly before original developers leave the organization.
Challenge 2: Data standardization inconsistencies
Healthcare data varies dramatically in structure and terminology across organizations. Medications, diagnoses, and procedures use different coding systems. Matching records across systems requires sophisticated data normalization.
How to overcome this challenge
- Implement terminology services that map between coding systems automatically during integration.
- Standardize on SNOMED, LOINC, and RxNorm for clinical concepts within telemedicine platforms.
- Build validation rules that flag data quality issues before transmission to downstream systems.
- Create master data management processes that maintain consistency across integrated applications.
- Invest in data governance programs that establish organizational standards for clinical documentation.
Challenge 3: Security and compliance requirements
Healthcare integration involves protected health information requiring strict security controls. HIPAA violations carry substantial penalties and reputational damage. Regulators scrutinize data exchange practices during audits.
How to overcome this challenge
- Encrypt all data transmissions using TLS 1.3 or equivalent strong encryption standards.
- Implement API authentication using OAuth 2.0 with short-lived tokens and refresh mechanisms.
- Conduct security assessments of integration partners before establishing data exchange connections.
- Maintain Business Associate Agreements with all vendors handling protected health information.
- Conduct regular penetration testing of integration endpoints to proactively identify vulnerabilities.
Challenge 4: Workflow disruption during implementation
Integration projects inevitably change how staff perform daily tasks. Resistance emerges when new workflows seem slower or more complex. Poor change management derails technically successful implementations.
How to overcome this challenge
- Involve clinical end users in the integration design to ensure workflows align with actual practice patterns.
- Pilot integrations with small user groups before organization-wide deployment begins.
- Provide comprehensive training that explains both technical changes and workflow improvements.
- Establish super-user programs where champions support colleagues during transition periods.
- Monitor adoption metrics and address concerns quickly before frustration spreads widely.
Challenge 5: Vendor coordination complexity
Telemedicine integration typically involves multiple vendors with different priorities and timelines. EHR vendors, telehealth platforms, and specialty systems all require coordination. Getting everyone aligned proves challenging.
How to overcome this challenge
- Designate integration project managers who own cross-vendor coordination responsibility.
- Establish regular multi-vendor status meetings with documented action items and deadlines.
- Define integration requirements in contracts before vendor selection to ensure capability.
- Use certified integration partners with proven experience connecting your specific systems.
- Build testing environments that enable vendors to collaborate safely on integration development.
Facing Telemedicine Integration Challenges?
Our healthcare integration specialists have solved these exact problems for hospitals, clinics, and digital health startups. We bring proven approaches that minimize risk and accelerate time-to-value.
Telemedicine Integration Cost Factors
Integration costs vary dramatically based on technical complexity and organizational requirements. Understanding cost drivers helps leaders budget appropriately and avoid surprises. Several key factors determine total investment.
Technical complexity factors
The systems being connected significantly impact development effort and timeline.
| Factor | Lower Cost | Higher Cost |
|---|---|---|
| Target EHR | Modern cloud EHR with FHIR APIs | Legacy on-premise system without APIs |
| Integration depth | Basic patient demographics | Full clinical workflow automation |
| Data volume | Hundreds of transactions daily | Millions of transactions daily |
| Real-time requirements | Batch synchronization acceptable | Sub-second response required |
| Security requirements | Standard HIPAA compliance | Additional certifications (HITRUST, SOC 2) |
Development approach impact
How organizations structure integration projects affects both cost and outcomes.
- Custom development provides maximum flexibility but requires significant investment. Teams build exactly what organizations need without compromise. Costs range from $75,000 to $300,000+, depending on scope.
- Integration platforms reduce development effort through pre-built connectors and tools. Platforms like MuleSoft, Microsoft Azure Integration Services, and healthcare-specific options accelerate delivery. Licensing costs add ongoing expense, but implementation moves faster.
- Vendor native integrations leverage built-in connectivity when available. EHR app marketplaces offer pre-certified telemedicine connectors. These options cost less but may limit customization flexibility.
Ongoing maintenance costs
Integration is not a one-time expense. Ongoing maintenance ensures continued operation and adaptation to changes.
- Monitoring and support require dedicated resources or contracted services. Someone must respond when integrations fail or performance degrades. Budget $2,000-$15,000 per month, depending on complexity.
- Upgrade management addresses changes when connected systems release new versions. EHR updates sometimes break existing integrations unexpectedly. Testing and remediation require ongoing investment.
- Enhancement requests inevitably emerge as users identify additional integration opportunities. The initial scope rarely captures all valuable use cases. Reserve budget for continuous improvement work.
Cost estimation framework
Organizations can estimate integration investment using this general framework.
| Integration Type | Typical Cost Range | Timeline |
|---|---|---|
| Basic EHR connectivity (demographics, scheduling) | $40,000 to $80,000 | 2 to 4 months |
| Comprehensive EHR integration (clinical data, orders, results) | $100,000 to $200,000 | 4 to 8 months |
| Multi-system integration (EHR + billing + pharmacy + labs) | $200,000 to $400,000 | 6 to 12 months |
| Enterprise integration platform | $300,000 to $750,000+ | 9 to 18 months |
Custom telemedicine platform development with full integration capabilities typically costs $150,000 to $300,000. ROI typically reaches 100% within six months through operational efficiencies.
Best Practices for Telemedicine Integration Success
Organizations that approach integration strategically achieve better outcomes with less disruption. These best practices emerge from successful healthcare integration projects. Apply them throughout your integration journey.
1. Define clear integration objectives
Start with specific, measurable goals rather than vague interoperability aspirations. Quantify current pain points and expected improvements. Business cases with concrete metrics drive appropriate investment.
Identify which workflow integration should be improved most urgently. Prioritize high-volume, high-impact processes over edge cases. Clinical and operational leaders should align on priorities.
Document success criteria before implementation begins. Everyone should agree on what “done” looks like. Post-implementation assessment becomes straightforward with predefined metrics.
2. Assess the current technical landscape thoroughly
Inventory all systems that integration will touch directly or indirectly. Document versions, configurations, and existing interfaces for each. Hidden dependencies often derail integration timelines.
Evaluate API availability and documentation quality for target systems. Some vendors provide excellent developer resources while others require extensive discovery. Understanding what exists informs realistic planning.
Identifying technical debt and modernization needs that might be integrated. Outdated systems sometimes cannot support desired integration patterns. Addressing prerequisites through telemedicine platform modernization prevents mid-project surprises.
3. Adopt healthcare interoperability standards
Build integrations on established standards like HL7 FHIR rather than proprietary approaches. Standards-based integrations adapt more easily as technology evolves. Organizations implementing FHIR report a 60% reduction in time required for new app integrations.
Leverage SMART on FHIR for application authorization and launch. This specification enables secure third-party application integration. Users benefit from seamless experiences within familiar EHR environments.
Plan migration paths from legacy standards where necessary. Many organizations still depend on HL7 v2 messaging. Hybrid approaches support current needs while enabling future modernization.
4. Implement robust testing protocols
Develop comprehensive test plans covering normal operations and edge cases. Integration testing must validate data accuracy, performance, and security. Production failures damage credibility and patient safety.
Create realistic test data that exercises all integration pathways. Synthetic patient records should include variations that stress boundary conditions. Testing with only simple cases misses important defects.
Establish staging environments that closely mirror production configurations. Integration testing in isolated sandboxes misses environmental issues. Pre-production validation catches problems before users encounter them.
5. Plan for scalability from the start
Design integrations that handle growth without architectural rework. Transaction volumes often exceed initial projections by a significant margin. Early scalability investment prevents expensive redesign later.
Implement asynchronous patterns when real-time responses are not required. Message queues handle load spikes gracefully without overwhelming target systems. Synchronous calls should be reserved for time-critical transactions.
Monitor integration performance continuously and establish capacity thresholds. Proactive scaling prevents degradation before users notice problems. Performance baselines enable trend analysis and prediction.
6. Establish governance and maintenance processes
Integration governance ensures ongoing oversight and continuous improvement. Someone must own integration health across organizational boundaries. Clear accountability prevents neglected integrations from failing silently.
Create runbooks documenting troubleshooting procedures for common issues. Support staff need guidance for resolving problems quickly. Well-documented processes reduce mean time to resolution.
Schedule regular integration reviews assessing performance, security, and alignment with current needs. Quarterly reviews identify optimization opportunities and emerging risks. Continuous attention maintains integration value.
Choose Space-O Technologies for Your Telemedicine Integration Project
Telemedicine integration transforms isolated virtual care tools into connected extensions of healthcare delivery. Organizations that invest in thoughtful integration achieve better clinical outcomes, operational efficiency, and patient satisfaction. The technical complexity requires experienced partners who understand both healthcare and modern software development.
Space-O Technologies brings 15+ years of healthcare software development expertise to telemedicine integration projects. Our healthcare developers hold HIPAA compliance certifications and understand the regulatory requirements affecting integration design. We have successfully connected telemedicine platforms with Epic, Cerner, athenahealth, and other major EHR systems. Integration projects benefit from our proven methodologies refined across 300+ software solutions.
Contact Space-O Technologies to discuss your telemedicine integration requirements. Our experts provide free consultations to assess your current landscape and recommend appropriate approaches. We deliver connected healthcare solutions that help you provide better patient care.
FAQs on Telemedicine Integration
What is the cost of telemedicine integration with EHR systems?
Telemedicine EHR integration typically costs between $40,000 and $200,000, depending on complexity. Basic demographic and scheduling integration falls toward the lower range. Comprehensive clinical integration with orders, results, and documentation increases costs. Organizations should budget additional amounts for ongoing maintenance and enhancement work.
How long does it take to implement telemedicine integration?
Implementation timelines range from 3 to 12 months, depending on the integration scope. Simple connectivity projects are completed in 3 to 4 months. Comprehensive multi-system integrations require 6 to 12 months. Discovery and requirements phases should not be rushed, despite pressure to deploy quickly. Thorough planning prevents costly rework during development and testing.
Which EHR systems support telemedicine integration most easily?
Major EHR vendors, including Epic, Cerner, and athenahealth, provide well-documented FHIR APIs for integration. Epic’s App Orchard marketplace offers certified telemedicine connectors. Cloud-based EHRs generally integrate more easily than on-premise legacy systems. Organizations should evaluate specific API capabilities before selecting telemedicine platforms.
What healthcare data standards should telemedicine platforms support?
Modern telemedicine platforms should support HL7 FHIR as the primary interoperability standard. SMART on FHIR enables secure application launch from within EHR systems. Legacy system connectivity may additionally require HL7 v2 messaging support. CDA documents effectively support the exchange of summary information between care settings.
Can telemedicine platforms integrate with remote patient monitoring devices?
Yes, modern telemedicine platforms commonly integrate with RPM devices, including blood pressure monitors, glucose meters, and wearables. Device data is transmitted to platforms using standards such as Bluetooth and cellular connectivity. Providers review trends during virtual consultations for chronic disease management. Integration requires careful attention to device certification and data accuracy.
Should organizations build custom integrations or use pre-built connectors?
The decision depends on specific requirements and available options. Pre-built connectors accelerate deployment when they align with organizational needs. Custom development offers flexibility for unique workflows and systems without relying on standard connectors. Many organizations combine approaches using pre-built components where possible and custom development where necessary.